Funded Research
Over the years The Radiological Research Trust has supported a large number of research projects in the field of imaging which have gone on to gain international awards in recognition of their achievements, large scale funding to further the research from organisations such as CRUK and The Wellcome Trust, as well as numerous papers and presentations being published to share the findings and learnings from the research with world wide audiences.
Some of the projects we have supported include:
MRI – Bone Mineral Density
Technical validation of a novel MRI technique for quantification of bone mineral density
Overview:
RRT funding enabled me to develop and build two imaging phantoms for technical validation of our methodology for measuring bone fraction. Each phantom had varying bone fractions (using calcium hydroxyapatite as a surrogate for bone). These phantoms were scanned and post-processed using our method. I was also able to carry out MRI scans on patients and compare these with CT scans acquired as part of their routine clinical care.
The RRT funding enabled me to get started with this project, the preliminary results of which have been presented at an international meeting and we hope will enable successful applications for further funding to develop the project.
The custom-built phantoms demonstrated viability of our method for measuring bone fraction using MRI. The MRI measurements (using our method) and reference bone fractions were compared using linear regression and demonstrated a significant relationship. We showed that our proposed method is sensitive to changes in bone fraction/bone mineral density over the range expected in human bone marrow.
This suggests that our method has clinical utility for disorders causing both new bone formation (i.e. increased bone fraction/bone mineral density) and bone destruction (i.e. reduced bone fraction/bone mineral density), such as spondyloarthritis and multiple myeloma.
Bone fraction/bone mineral density images were generated from the MRI scans of subjects and compared with CT scans acquired as part of routine care, demonstrating proof-of-principle in vivo.
- Poster presentation at the International Society of Magnetic Resonance in Medicine (ISMRM) 2019 annual meeting in Montreal “Bone Fraction Mapping with SyNthetic Auto-interpolated in-Phase (SNAP) MRI”
- Awarded a stipend to attend the ISMRM workshop on MRI of obesity and metabolic disorders (July 2019)
- Results to be written up as a paper ans submitted to a peer reviewed journal
- Future funding application planned to continue this work and compare with current clinical standard (DEXA)
This is an excellent funding opportunity to start a new project. Discuss your project with supervisors and make sure you have the necessary technical support e.g. medical physicist, radiographers.

MRI – Juvenile Idiopathic Arthritis
Quantitative magnetic resonance imaging in juvenile idiopathic arthritis
Overview:
RRT funding enabled me to develop and build two imaging phantoms for technical validation of our methodology for measuring bone fraction. Each phantom had varying bone fractions (using calcium hydroxyapatite as a surrogate for bone). These phantoms were scanned and post-processed using our method. I was also able to carry out MRI scans on patients and compare these with CT scans acquired as part of their routine clinical care.
The RRT funding enabled me to get started with this project, the preliminary results of which have been presented at an international meeting and we hope will enable successful applications for further funding to develop the project.
The custom-built phantoms demonstrated viability of our method for measuring bone fraction using MRI. The MRI measurements (using our method) and reference bone fractions were compared using linear regression and demonstrated a significant relationship. We showed that our proposed method is sensitive to changes in bone fraction/bone mineral density over the range expected in human bone marrow.
This suggests that our method has clinical utility for disorders causing both new bone formation (i.e. increased bone fraction/bone mineral density) and bone destruction (i.e. reduced bone fraction/bone mineral density), such as spondyloarthritis and multiple myeloma.
Bone fraction/bone mineral density images were generated from the MRI scans of subjects and compared with CT scans acquired as part of routine care, demonstrating proof-of-principle in vivo.
- Poster presentation at the International Society of Magnetic Resonance in Medicine (ISMRM) 2019 annual meeting in Montreal “Bone Fraction Mapping with SyNthetic Auto-interpolated in-Phase (SNAP) MRI”
- Awarded a stipend to attend the ISMRM workshop on MRI of obesity and metabolic disorders (July 2019)
- Results to be written up as a paper and submitted to a peer reviewed journal
- Future funding application planned to continue this work and compare with current clinical standard (DEXA)
This is an excellent funding opportunity to start a new project. Discuss your project with supervisors and make sure you have the necessary technical support e.g. medical physicist, radiographers.

MRI – Prostate haemorrhage
MRI – Post-biopsy prostate haemorrage and its effect on prostate MRI
Overview:
The current practice for men with increased PSA and suspicious of prostate cancer is ultrasound guided biopsy (TRUS) to obtain tissue confirmation, followed by multi-parametric MRI of prostate to localise the tumour.
However, the biopsy procedure itself causes haemorrhage in prostate tissue, which can hinder MRI ability to localise significant cancer. This is mainly due to resemblance of signal characteristics of haemorrhage to cancer on prostate MRI.
In this work, we prospectively analysed the signal characteristics of the entire volume of prostate on different MRI components (T1, T2-weighted and diffusion MRI) before and at 1,2 and 6 months after biopsy in 14 men with negative prostate MRI (i.e. no prostate cancer visible on MRI).
Our results suggest that quantitative MRI signal changes following biopsy remain even after 6 month. We also showed that the most reliable quantitative MRI metrics following biopsy is apparent diffusion coefficient (ADC) from diffusion MRI. ADC in our analysis showed no significant changes across the entire volume of prostate at any time point.
Our results have two important clinical implications. Firstly, it emphasise the importance of organising MRI scans prior to prostate biopsy. This is more relevant with emergence of techniques such as template mapping biopsy (TMP) where increasing number of samples is acquired from prostate tissue.
Secondly, if MRI exam is performed after biopsy, ADC measurement may aid in localisation and characterisation of suspected tumour.
ADC is known to significantly decrease in prostate tumour when compared to normal prostate tissue and since its value is not affected by presence of haemorrhage, it can be reliably used even at 1 month following biopsy.
MRI – Professional Footballers Injuries
Using MRI to study a range of clinical injuries incurred by footballers.
Overview:
A Grant from the Radiological Research Trust collaboratively with both the Football Association and The Professional Footballers’ Association funded research utilizing MRI to look at and study a range of clinical injuries incurred by footballers.
Studies particularly looked at Anterior Cruciate Ligament and Posterior Cruciate Ligament deficiency and reconstruction on the kinematics of the knee. Research included a dynamic MRI analysis of tibiofemoral motion looking at the Lachman test for the diagnosis of rupture of the anterior cruciate ligament.
MRI – Paediatric Lymphoma
Whole body MR imaging for the staging of paediatric lymphoma.
Overview:
Funding provided research into whole body MR imaging for the staging of paediatric lymphoma allowing the creation of an MRI protocol that was acceptable to children and adolescents and determined its accuracy for lymphoma detection and staging compared to the current standard clinical care.
This proof of concept work showed that Whole Body MRI is a viable alternative to radiation heavy imaging techniques that have been typically used.
This has enabled the group to go on to achieve CRUK funding for a prospective trial in childhood lymphoma and Great Ormond Street Hospital Charity funding for an offshoot trial evaluating combining the techniques developed with Positron Emission Tomography in PET-MR. Without the RRT pump priming, these larger projects and greater level of funding would not have been possible.
MRI – Childhood Lymphoma
Development of MRI for whole-body assessment of disease as an alternative to conventional methods utilizing ionising radiation.
Overview:
Lymphoma is staged using the Ann Arbor classification which relies upon a combination of clinical symptoms and accurate assessment of extent of lymph node involvement. Conventional staging procedures include biopsies, radiography, computed tomography (CT) and ultrasound. CT has been the gold standard of staging lymphoma but provides only structural information. Although CT has excellent spatial resolution, disease is only assessed based on size criteria, with lymph nodes less than 1 cm considered as not involved. Positron Emission Tomography (PET) using 18FDG adds information on the metabolic activity of the involved nodes and has increasingly been incorporated into the staging investigations in lymphoma patients. This functional information can also be particularly useful in determining response to therapy. Both CT and PET use ionising radiation and it is known that exposure to even small doses of ionising radiation is associated with a risk of development of second cancers. With disease having to be restaged at several intervals during a treatment regimen a substantial cumulative dose of radiation can be imparted to the patient as a result of the imaging investigations. The effect of this radiation exposure is of greater concern in the setting of childhood lymphoma where the relatively longer lifespan of a child allows more time for a consequential development of malignancy to manifest. Imaging techniques that allow accurate staging of disease whilst reducing exposure to ionising radiation would be of great benefit in this population. Magnetic resonance imaging with its ability to provide both accurate anatomical images and a variety of functional imaging contrasts using non-ionising radiation has the potential to perform the role of the ‘ideal’ imaging modality. This study will compare anatomical and functional information obtained using MRI with that obtained with the current standard conventional imaging techniques of PET and CT in children and adolescents with lymphoma. MRI will be performed in addition to the routine PET and CT investigations at initial staging and restaging following chemotherapy. The ability of MRI to monitor and assess patient response to chemotherapy will be determined.
Primary Study Aims:Compare whole body MRI to anatomical CT and functional PET imaging in childhood lymphoma preceding chemotherapy treatment.Correlate functional MR imaging at time of diagnosis (diffusion, perfusion and oxygenation dependent contrast images) with PET/CT data of active tumour tissue.Investigate whether functional MRI changes during chemotherapy treatment can predict ultimate clinical response after a full course of treatment.Secondary Study Aims:
Compare MRI, CT and PET/CT characteristics of imaging classified abnormal lymph nodes with histology obtained by routine diagnostic biopsy.
Investigate the change in imaging findings during treatment for different histologically classified disease types.
MRI – Teenage Brian Tumours
Assessment of the structure and function of brain tumours in teenagers using MRI before and following treatment.
Overview:
Gliomas account for approximately 50% of all brain tumours in the adolescent and young adult population. Although most of these patients have an excellent outcome, a small but significant proportion will either relapse or experience tumour progression after definitive treatment. The traditional and accepted criteria to determine tumour response in oncology, namely the Response Evaluation Criteria in Solid Tumours (RECIST) and Macdonald criteria, use decrease in tumour size and lesion enhancement as an indicator of successful therapy. As more aggressive combined modality treatments are being investigated for the management of gliomas, it has become increasingly important to identify earlier indicators of regional response or regression. This would enable earlier initiation of effective treatment options, and thereby optimize patient outcome.
Although considerable work has been done in this area using CT in body tumours, several areas within the field of MRI have seen considerable advances making MRI an ideal tool: modern contrast media, advanced morphologic approaches and several functional techniques, in the visualization of tumour perfusion or tumour cell metabolism. Proton magnetic resonance spectroscopy (MRS) allows the non-invasive detection of brain metabolites. Increasing lactate to creatine and choline to creatine levels are associated with tumour recurrence in adult gliomas, noted before progression on conventional neuroimaging. MRI perfusion characterizes tumour vasculature and has been shown to correlate with tumour grade. Recent studies have demonstrated the value of this technique in predicting survival in high-grade gliomas during radiotherapy and as an imaging biomarker for early cancer outcome. Diffusion weighted imaging (DWI) assesses free water movement in tissues and a recent study in glioblastoma multiforme treated with bevacizumab has shown that the Apparent Diffusion Coefficent (ADC) of tumours prior to treatment can stratify progression-free survival.
The success or failure of new and/or augmented treatments will be closely linked to appropriate patient selection. Fortunately, the clinical proliferation of “functional” MRI capable scanners and techniques provides an opportune time for the development of new and likely improved patient stratification methods. Our study will assess a multitude of functional MRI features in order to determine those that are predictive of tumour response to chemoradiotherapy. In addition, we will establish the ranges of these parameters found in disease, which could lead to potential improvements in imaging diagnosis of glioma.
Finally, an important correlation to imaging and clinical outcome data will be the histological phenotype and the molecular profile of the brain tumour. It will be key to improving clinical management and ultimately patient survival.
Primary Study Aims:To evaluate whether pre-chemoradiotherapy and/or early post-chemoradiotherapy functional MRI features (diffusion, dynamic contrast enhancement, spectroscopy and blood oxygenation level dependent contrast) can predict subsequent tumour response in adolescents/young adult patients with glioma.
Secondary Study Aims:To identify the ranges of individual functional MRI parameters associated with the presence of disease prior to and following treatment.
MRI – Lung Cancer
Assessment of the structure and function of lymph nodes within the chest using MRI in patients with known lung cancer.
OVERVIEW:
Lung cancer is the biggest cancer killer in the UK, accounting for more than one in five cancer deaths.
Accurate staging of non-small cell lung cancer is the critical step which determines both the treatment modality and the prognosis. This is currently best accomplished via a multidisciplinary approach involving surgical, respiratory, oncology and radiology input in order to establish whether or not curative surgical resection is possible. Preoperative mediastinal lymph node staging separates initial operative versus non-operative status. Patients without mediastinal nodal metastases (or occasionally with ipsilateral nodes) are considered operative candidates, while patients with central or contralateral mediastinal nodal metastases are treated primarily with chemotherapy and external beam radiotherapy.
Several invasive and non-invasive methods exist to diagnose and stage lung cancer, and most patients require more than one. Inadequate staging or indeed incorrect staging of the mediastinal nodes can have the catastrophic consequences of a missed opportunity to operate or more commonly an inappropriate operation leading to high morbidity and worse outcome.
The limitations of CT in assessing nodal disease are highlighted by a false positive rate of 40% in mediastinum and the fact that 5 to 15% of patients with clinical T1N0 (stage I) tumours are found to have positive lymph node involvement at surgery. Therefore CT can overstage and understage and cannot solely determine mediastinal lymph node status in patients with NSCLC.
Sensitivity and specificity of PET for identifying mediastinal metastasis have been reported to be 74% (95% CI, 69 to 79%) and 85% (95% CI, 82 to 88%) respectively.
Recent advances in Magnetic Resonance Imaging provide the opportunity to accurately image the mediastinum with little if any respiratory or cardiac motion artefact. At UCLH we already have experience in this area with our work on the staging of paediatric lymphoma. In addition to hi-resolution anatomical imaging MRI can give a functional assessment of small nodes that are deemed not to be diseased by CT size criteria, and is therefore could prove more sensitive and specific than CT.
Patients with known lung cancer and mediastinal nodes on CT undergo endoscopic ultrasound (EBUS) guided biopsies of mediastinal nodes as small as 0.5 cm in diameter. This pilot study will determine if it is possible to accurately detect nodal involvement using MRI by comparing multi-parametric MR characteristics of lymph nodes with EBUS nodal biopsies.
Primary Study Aims:Evaluate the anatomical and functional MRI characteristics of mediastinal nodes by correlation to a histological gold standard obtained from EBUS guided biopsies for patients with lung cancer.Compare MR imaging and contrast enhanced chest CT data in assessing mediastinal nodal disease.
Secondary Study Aims:Investigate whether respiratory and cardiac gated hi-resolution MRI is able to detect lung disease in patients with CT diagnosed lung cancer.
MRI – Fluoroscopy
A feasibility study to determine the relationship between disc degeneration and inter-vertebral motion using open upright MRI and quantitative fluoroscopy
Overview:
Introduction: Disc degeneration (DD) has been linked to low back pain (LBP) and studies suggest that DD affects inter-vertebral motion, but the link between altered inter-vertebral motion and LBP is still unknown. The current standard of measuring inter-vertebral motion is functional radiography (flexion extension radiographs) however these only measure end of range motion and do not give dynamic information, nor information regarding the state of the inter-vertebral disc.
The Radiological Research Trust supported a feasibility study to determine the optimum methods of combining two new imaging techniques to investigate the relationship between inter-vertebral motion and DD in healthy volunteers as a pre-cursor to a larger grant application to investigate the same in patients with LBP. The two imaging techniques are quantitative fluoroscopy (which can objectively measure dynamic inter-vertebral motion) and open upright MRI which can determine the state of the inter-vertebral disc under load.
Healthy participants (n=10) were recruited and underwent both procedures in supine and weight-bearing positions at the Anglo-European College of Chiropractic in Bournemouth. The feasibility study determined the acceptability of the procedures to participants and the level of data needed (collection and analysis) to determine the existence of relationships between inter-vertebral motion and DD in the lumbar spine.
The results shaped the protocol for the main study, and are currently in preparation for publication. They were presented at local conferences, including the Council for Allied Health Professions Research (CAHPR) Southampton Hub, and the Anglo-European College of Chiropractic research feedback event.
Ultrasound – Crohn’s Disease
Can Ultrasound using microbubbles as contrast detect and monitor changes in areas of inflammed bowel in patients with Crohn’s disease?
Overview:
Crohn’s disease is a chronic inflammatory condition of the bowel, predominately affecting the young and requiring lifelong medical and often surgical therapy. The natural history of the disease is one of intermittent acute exacerbations characterised by an acute inflammatory response, separated by periods of relative quiescence. Medical therapy is based largely on immunosuppressive medication. Although relatively effective, these drugs are not without significant side effects, some of them life threatening, notably sepsis secondary to immunosuppression. Newer immuno-modulating agents such as anti-TNF medication have been shown to be effective in patients with severe disease refractory to first line therapy. However two weeks after initial treatment only around 50-60% of recipients respond to anti TNF therapy, a figure dropping to below 50% after 30 weeks, despite repeated dose. Furthermore such agents are expensive, require intravenous or subcutaneous administration and are not without additional significant side effects including anaphylaxis, and fatal infections, and have been linked to future malignancies, particularly lymphoma.
Rational use of such immunosuppressive therapies in Crohn’s disease therefore relies on accurate identification of those patients who will benefit most from treatment. In routine clinical practice, anti-TNF therapy is often administered initially over 3 doses, each separated by two to four weeks, with patients usually undergoing a full 6 weeks course before a final judgement is made regarding treatment efficacy. At the present time this judgement is usually made by assessing the clinical response of patients using symptom based questionnaires such as the Crohn’s disease activity index. Such clinical assessments based on patient symtomatology are relatively subjective, and patients with inactive disease (such as those with chronic fibrotic strictures) often attract high scores. Biochemical markers such as ESR and CRP are useful adjuncts but again do not in themselves always correlate with disease activity.
Ideally it would be possible to predict which patients with luminal Crohns disease will respond to anti-TNF therapy before the medication is given. However even if an accurate judgement of efficacy could be made after the first dose of medication, this would be a significant advantage, potentially sparing non-responders a further two doses from which they are destined to receive no benefit. In the absence of an external marker such as active entero-cutaneous fistula, neither clinical assessment nor biochemical markers are sufficiently accurate to make this early assessment, but radiological techniques notably MRI and ultrasound hold considerable promise as alternatives.
It is known that active Crohn’s disease is associated with changes in mural vascularity and assessment of mural blood flow using Doppler ultrasound has been shown to correlate with disease activity. However, although subjective assessment of mural vascularity using Doppler is simple, the technique is somewhat limited due to relatively low blood flow within bowel wall, which may be undetectable using conventional Doppler ultrasound settings, even if pathologically increased.
Intravenously administered ultrasound contrast agents are widely used in routine radiological practice to improve the detection and characterisation of vascular phenomena within various organs, including the small bowel. Such agents consist of tiny “microbubbles” which augment the Doppler signal of flowing blood and increase the sensitivity of Doppler ultrasound in low flow states. The agents, which have a proven safety record, enter the vascular pool after intravenous administration before being excreted via the lungs after a few minutes. New analysis software also now also allows quantification of mural blood flow within a defined region of interest.
The purpose of this study will be to measure and quantify changes in bowel wall blood flow using contrast enhanced ultrasound in patients with active Crohn’s disease undergoing Infliximab therapy, and assess whether measured changes can predict ultimate response to treatment.
Primary Study Aims:
Using anatomical and contrast-enhanced ultrasound, document and quantify the effect of anti-TNF medication on mural morphology and blood flow.Correlate anatomical and contrast-enhanced ultrasound derived changes in mural morphology and blood flow with clinical and biochemical markers of response to anti-TNF medication.Investigate whether contrast-enhanced ultrasound derived changes in mural blood flow can predict ultimate clinical response to medication.
Secondary Study Aims:
Re-affirm the correlation between anatomical and contrast-enhanced ultrasound derived changes in mural morphology and blood flow with clinical and biochemical markers of disease activity.Investigate whether anatomical and contrast-enhanced ultrasound derived mural morphology and blood flow before commencement of anti-TNF therapy can predict ultimate clinical response.
MRI – Juvenile idiopathic arthritis
Quantitative MRI in juvenile idiopathic arthritis
Overview:
Juvenile idiopathic arthritis (JIA) is the most common form of arthritis in children and adolescents, and is a significant cause of morbidity. Enthesitis-related arthropathy (ERA) is a disease subtype with particularly poor outcomes: compared to other subtypes, ERA patients experience poorer long term physical health and more disability. The disease is also notoriously difficult to assess clinically due to the fluctuating nature of the disease and the fact that adolescents are poor reporters of pain. The sacroiliac joints are also deep and difficult to palpate.
There is a clear need for objective markers of joint inflammation to inform therapeutic decision-making. In addition, accurate and early diagnosis could facilitate earlier and more effective treatment and may reduce long-term morbidity.
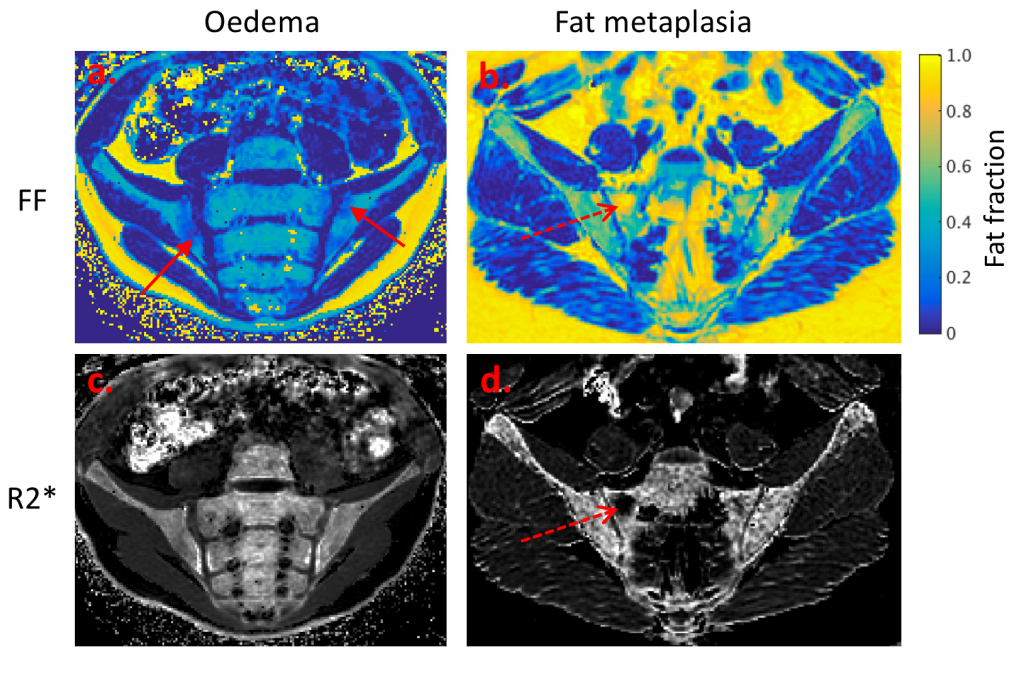
RRT funding allowed the researchers to develop and optimize an MRI scan protocol for measuring the fat fraction of the sacroiliac joints as a measure of joint inflammation. Both ‘online’ and ‘offline’ methods were developed to process the raw imaging data using a variety of techniques, which are undergoing continuous refinement and improvement.
Technical and preliminary biological validation of fat fraction as an inflammatory biomarker was undertaken. Specifically, showing that fat fraction measurements are highly repeatable (with an intraclass correlation coefficient of approximately 0.98). A novel fat-water phantom was constructed and used to demonstrate the accuracy of fat fraction measurements using a 3T Philips Ingenia scanner. Sixteen patients with enthesitis-related arthritis were scanned and preliminary data suggested that agreement with conventional radiological measures is excellent. Patient recruitment is still ongoing.
X-Ray – Visual acuity
The impact of reduced visual acuity for the detection of lesions in mammography
Overview:
Visual acuity reduces with age; it also becomes worse at the end of a long radiology workday. However, the impact of this reduction in visual acuity on diagnostic decision-making is not well understood and it has not been given much attention in radiological research. The aim of this funded study was to assess the impact of reduced visual acuity on the detection of lesions in breast screening images.
X-Ray/MRI – Spinal structure and range of motion under load bearing conditions
The effect of 8 hr axial active load bearing on spinal structure, laxity and range of motion via MRI and quantitative fluoroscopy when supine and standing
Overview:
The project aim was to investigate the effect of 8 hour (occupational) true vertical loading on the structure and mobility of the spine. MRI scans were performed while subjects were lying down as usual and were compared with scans during which they were sat upright. The hypothesis being that an upright scan may be more appropriate when investigating loading-induced issues in the spine. In addition, by evaluating a new form of X-ray fluoroscopy the project helped to determine the relationship between structural changes and the laxity of the spine and its range of movement, both of which are measures that radiologists and clinical practitioners require in order to evaluate axial load-induced dysfunction, loss of stature and/or pain.
MRI – Super-resolution for magnetic resonance cholangio-pancreatography
Super-resolution for magnetic resonance cholangio-pancreatography
Overview:
Two-dimensional MRI scans allow different tissues to be seen clearly, but image slices are thick and can miss out important findings between slices. Super-resolution combines information from previously acquired images obtained in different planes to create a new high resolution thin-slice volume but with preserved tissue differences. Funding provided supported the implementation of a novel application of super-resolution to upper abdominal MRI where many tightly packed structures are often inadequately imaged using current techniques. The technique was applied in normal volunteers as a pilot study to support the translation of this approach to patient cohorts, ultimately improving patient care by improving the diagnostic yield of abdominal MR techniques.
MRI – Hyperpolarised MRI
Metabolic Imaging in Renal Cancer using hyperpolarised MRI
Overview:
RRT provided funding support the development of a rapid imaging protocol for hyperpolarised MRI. The MRI pulse sequence validation was carried out on phantms and the clinical imaging protocol was optimised in healthy volunteers. The developed protocol has since been utilised to probe in–vivo tumour metabolism in prostate cancer patients. Identification of aggressive tumour types by their metabolic signature could be used to plan treatments and prevent unnecessary surgeries. These developments have enabled the first acquisition of hyperpolarised MRI data in a cohort of prostate cancer patients in Europe and will form the basis of future grant applications.
MRI – Placental function
Advanced MRI for the assessment of placental function in Fetal Growth Restriction
Overview:
Poor placental vascularisation (placental insufficiency) leads to inadequate exchange of oxygen and nutrients between mother and fetus. Placental insufficiency underlies the major obstetric syndromes of fetal growth restriction and pre-eclampsia and accounts for one third of stillbirths in high-income countries. Currently existing imaging modalities provide poor clinical assessment of placental perfusion, function and pregnancy outcome.
The RRT funding supported a team who had developed an MRI method to measure both fetal and maternal placental perfusion. MRI data was acquired from appropriately grown and growth-restricted pregnancies, to quantify placental perfusion and determine its utility to predict maternal and neonatal outcome.